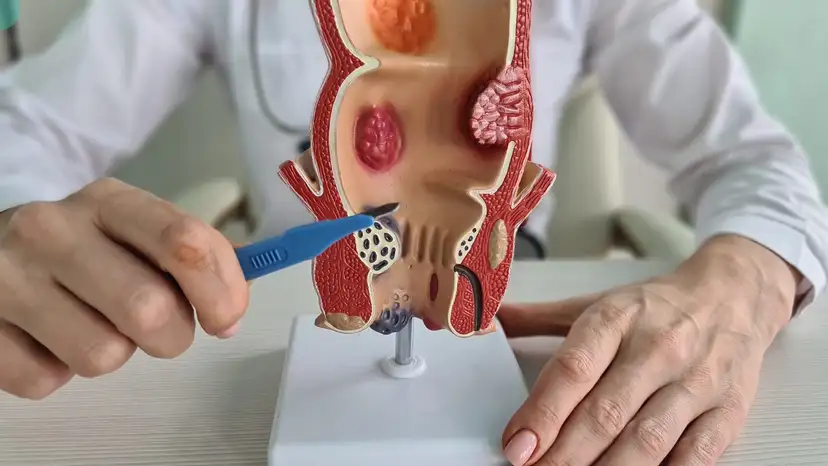
Anal fistulas are abnormal connections that form between the inner lining of the anal canal and the skin surrounding the anus. These fistulas typically develop following a perianal abscess, which is a localized infection that creates a pocket of pus. Without proper treatment, anal fistulas can lead to chronic pain, recurring infections, and significant discomfort during daily activities. Recognizing the symptoms early, such as persistent drainage, irritation, and occasional bleeding, is essential for seeking timely medical care. Anal fistulas are often challenging to manage due to their tendency to recur if inadequately treated. Surgical intervention is frequently necessary to ensure complete healing. Among the available surgical options, sphincterotomy has proven to be particularly effective in promoting recovery while minimizing complications.
Sphincterotomy is a surgical procedure designed to relieve pressure within the anal canal and promote proper drainage of the fistula tract. It is commonly performed in cases where the fistula involves part of the anal sphincter, allowing controlled access for repair. The goal is to facilitate the healing process by ensuring that any trapped pus or infection can drain effectively. This procedure may be performed alongside other fistula repair techniques, such as fistulotomy or fistulectomy, depending on the fistula’s complexity and location. By carefully cutting a portion of the sphincter muscle, surgeons reduce the tension that can hinder healing. Despite concerns about potential incontinence, when performed by an experienced surgeon, sphincterotomy usually preserves sphincter function. Patients often experience faster recovery times and improved outcomes compared to non-surgical approaches.
Understanding How Sphincterotomy Promotes Healing
The primary mechanism through which sphincterotomy supports healing is by relieving internal pressure and allowing the fistula tract to drain naturally. When pus or fluid accumulates in the fistula, it can exacerbate inflammation and pain, slowing recovery. Sphincterotomy enables consistent drainage, reducing the risk of recurrent abscess formation. The procedure also encourages the surrounding tissue to heal gradually from the base outward, promoting more complete closure of the fistula tract. By addressing the root cause of pressure buildup, sphincterotomy prevents repeated flare-ups and decreases the likelihood of infection. In addition, patients often notice a reduction in swelling and discomfort shortly after the procedure. The controlled cutting of the sphincter allows surgeons to maintain continence while providing a clear pathway for healing. Proper post-operative care, including hygiene and dietary adjustments, further supports recovery.
Advantages of Sphincterotomy in Anal Fistula Management
Sphincterotomy provides several notable benefits for individuals seeking long-term relief from anal fistulas. Patients typically experience faster healing times and lower recurrence rates compared to conservative treatments. Pain and swelling are reduced, and the fistula tract can close more effectively. The controlled nature of the procedure ensures that the risk of sphincter damage is minimized. Other advantages include:
- Efficient drainage of abscesses and infected material
- Reduced inflammation in surrounding tissue
- Minimal disruption to daily activities during recovery
- Improved quality of life and comfort
- Support for additional surgical procedures if needed
- Lower likelihood of chronic fistula recurrence
These benefits make sphincterotomy a preferred method for complex fistulas or fistulas that have not responded to non-surgical treatments. Proper patient selection and surgical expertise are critical to maximizing these positive outcomes.
Recovery Process After Sphincterotomy
Recovery following sphincterotomy requires a combination of proper wound care, lifestyle adjustments, and careful monitoring. Patients can expect some discomfort and mild bleeding during the first few days after surgery, which typically improves with pain management strategies prescribed by the physician. Maintaining proper hygiene is essential, including gentle cleaning of the anal area and avoiding irritants that could slow healing. Dietary modifications, such as increasing fiber intake and staying hydrated, can help prevent constipation, which may place additional pressure on the surgical site. Routine follow-up visits allow the surgeon to monitor progress and address any complications promptly. The average recovery period varies, but many patients return to normal activities within several weeks while full tissue healing may take longer. Avoiding heavy lifting or straining during the early stages is crucial to prevent setbacks. By following these post-operative care instructions, patients support the long-term success of anal fistula repair and removal.
Risks and Considerations
While sphincterotomy is generally safe, it carries some potential risks that patients should consider. These include bleeding, infection, and in rare cases, incontinence if the sphincter is overly compromised. The likelihood of complications increases with more complex or recurrent fistulas. Individual factors such as age, overall health, and previous surgeries can also affect outcomes. Surgeons carefully evaluate each case to determine the extent of sphincterotomy required. Patient adherence to post-operative care instructions significantly influences the healing process. Discussing concerns and expectations with the surgeon before the procedure ensures that patients are fully informed about potential risks and benefits. Understanding these considerations helps patients make confident decisions regarding their anal fistula repair and removal.
Complementary Therapies and Ongoing Care
In addition to the surgical procedure, several complementary therapies can aid recovery and enhance outcomes. Antibiotics may be prescribed to control infection, while topical treatments can reduce inflammation and discomfort. Pelvic floor exercises or physiotherapy can strengthen sphincter muscles, improving function and minimizing complications. Regular check-ups allow healthcare providers to track healing progress and identify any early signs of recurrence. Maintaining proper bowel habits, staying hydrated, and following a high-fiber diet support long-term anal health. Lifestyle modifications, including avoiding prolonged sitting and heavy lifting, further protect the surgical site. Combining these strategies with sphincterotomy ensures a comprehensive approach to managing anal fistulas effectively.
Frequently Asked Questions (FAQ)
Can sphincterotomy completely cure an anal fistula?
Sphincterotomy can effectively promote healing and reduce recurrence rates, but the success depends on fistula complexity and adherence to post-operative care. Some cases may require additional procedures.
Is sphincterotomy painful, and what anesthesia is used?
The procedure is typically performed under local or general anesthesia, ensuring minimal discomfort during surgery. Post-operative pain is manageable with prescribed medications.
How long does it take to recover fully after sphincterotomy?
Most patients can resume daily activities within a few weeks, but complete tissue healing may take several months. Recovery timelines vary depending on the individual.
What is the risk of incontinence after sphincterotomy?
When performed by an experienced surgeon, sphincterotomy preserves continence in the majority of cases. Risk increases with extensive muscle involvement.
Are there alternatives if sphincterotomy is not suitable?
Alternatives include fistulotomy, seton placement, or advanced minimally invasive techniques. The best option depends on fistula location and severity.
Can anal fistulas recur after sphincterotomy?
While recurrence is less common with proper treatment, it can still occur, especially in complex or untreated underlying infections. Follow-up care reduces this risk.
How should I care for the wound after the procedure?
Wound care involves gentle cleaning, using sitz baths, and avoiding strain or pressure on the surgical site. Adhering to physician instructions ensures optimal healing.
Takeaway
Sphincterotomy plays a critical role in supporting successful healing of anal fistulas. By relieving pressure, promoting drainage, and facilitating tissue repair, the procedure addresses the underlying causes of fistula formation. Combined with proper post-operative care, complementary therapies, and careful monitoring, sphincterotomy offers a reliable path to recovery. Patients benefit from faster healing, reduced pain, and lower recurrence rates, making it a preferred option for complex anal fistulas. Understanding the procedure, recovery process, and ongoing care ensures informed decisions and improved quality of life for those affected.